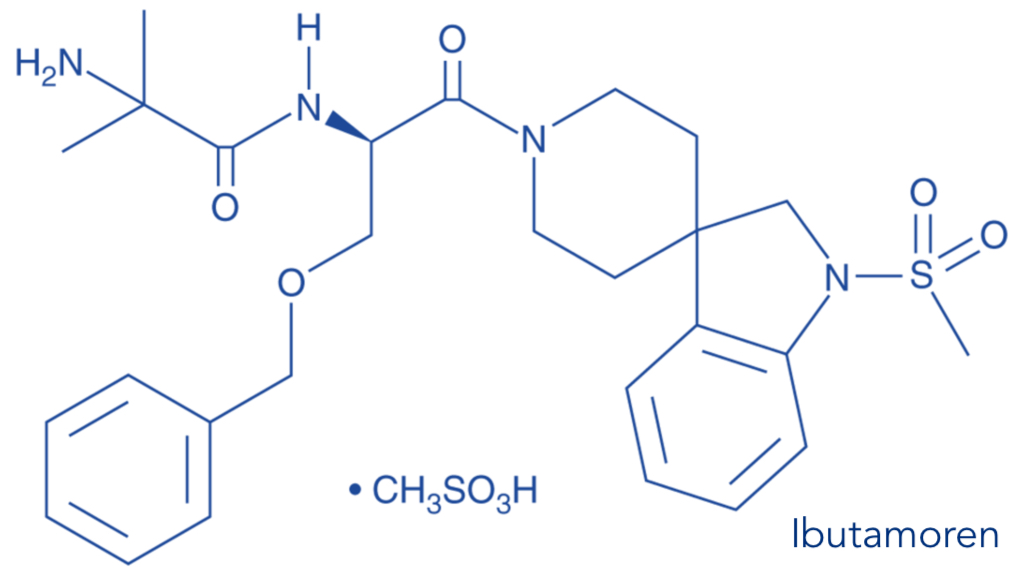
LUM-201, also known as ibutamoren, is an investigational, once-daily, orally administered small molecule that promotes the secretion of Growth Hormone (GH) from the pituitary gland.
LUM-201 has been observed to increase the amplitude of endogenous pulsatile GH secretion, which mimics the natural pattern of GH secretion via potent agonism of the growth hormone secretagogue receptor. Click on the video below to learn more about LUM-201’s Mechanism of Action in Pediatric Growth Hormone Deficiency (PGHD).
LUM-201 has been studied in more than 1300 patients (more than 150 children) and was generally well-tolerated.*
*IMPORTANT SAFETY INFORMATION: LUM-201 has a favorable investigational safety profile to date. LUM-201 was generally well-tolerated in children with the most commonly reported adverse events being increased appetite, pain in extremity and arthralgia. No meaningful safety signals have been observed in laboratory values, adverse events data, or in EKG values to date- Phase 2 Trials OraGrowtH210 and 212 Safety Data as of March 2024 cut-off date.
LUM-201 FOR PEDIATRIC GROWTH HORMONE DEFICIENCY (PGHD)
WHAT IS PEDIATRIC GROWTH HORMONE DEFICIENCY (PGHD)?
Growth hormone (GH) deficiency is the consequence of inadequate secretion of growth hormone from the pituitary gland. This results in low GH in the body, insufficient production of downstream signaling molecules required for growth, and the subsequent lack of growth. In children, this rare disorder is called pediatric growth hormone deficiency (PGHD).
Secretion of GH is under strict hormonal feedback control. Growth hormone-releasing hormone (GHRH) and ghrelin are stimulators of GH production, while somatostatin activity inhibits GH production.
GH is an important hormone regulating growth in childhood and adolescence.
CAUSES OF PGHD
PGHD can be congenital (children are born with the condition), acquired (brain tumor, head injuries or other causes), iatrogenic (induced by treatment for cancer), or idiopathic (of unknown cause). Consequences of PGHD can range from severe to moderate.
WE BELIEVE LUM-201 HAS THE POTENTIAL TO
IMPROVE THE LIVES OF PATIENTS WITH PGHD
DIAGNOSTIC PROCESS
In children, PGHD results in and manifests as slower-than-normal growth. Children are usually diagnosed by approximately seven years of age due to short stature and stunted growth velocity, although some children are not diagnosed until delay in pubertal growth spurt. About 1 in 3500 children are diagnosed with PGHD.3
PGHD is generally diagnosed by clinical observations and multiple tests, including radiographic assessment of bone age and tests of other hormones.
GH release stimulation tests are often needed to confirm PGHD diagnosis.
PGHD TREATMENT
Current treatment options are limited to injectable formulations (daily or weekly) of recombinant human growth hormone (rhGH). Treatment should be started as soon as PGHD diagnosis is confirmed. Long-term (seven years or longer) treatment is not uncommon to achieve “catch-up” growth and reach full height potential. Unfortunately, any routine injection can be painful, potentially leading to missed doses and sub-optimal growth.1,2
Treatment response is assessed by measurement of height and growth velocity. Treatment is usually continued until final height, completion of skeletal bone maturation (epiphyseal closure), or both have been recorded.
The main therapeutic goal of growth hormone treatment in children with PGHD is to enable these children to achieve normal height, with accompanying improvement of the psychosocial problems related to short stature.
LUM-201 PREDICTIVE ENRICHMENT MARKER STRATEGY (LUM-201 PEM) FOR PGHD
A Predictive Enrichment Marker (PEM) strategy uses clinical markers to identify patients who are likely to respond to a given treatment of a disease or condition. Often there will be two groups of responders according to specific criteria: positive responders and negative responders. A PEM strategy is typically applied when a disease has a variety of causes, resulting in varied responses to available treatments.
The LUM-201 Predictive Enrichment Marker Strategy (LUM-201 PEM) uses two common laboratory tests to help predict if a child is more likely to respond to oral investigational LUM-201 therapy (PEM positive/PEM+) or less likely (PEM negative/PEM-). The two tests are a pre-dose blood sample to evaluate baseline IGF-1 levels and post-dose blood sample to evaluate the GH response to a single oral dose of LUM-201. LUM-201-PEM findings help to understand if investigational oral LUM-201 potentially helps stimulate the child’s own hypothalamic/pituitary gland to increase their own endogenous GH secretion.
Pediatric Growth Hormone Deficiency (PGHD) has a number of different causes; not all patients will benefit from treatment with LUM-201. The Lumos Pharma OraGrowtH Trials Program uses the LUM-201 PEM Strategy to screen children to enroll in our clinical trials.
Drawing from LUM-201 data that had previously shown to increase the pulsatile release of growth hormone in healthy adults and adults with Growth Hormone Deficiency (GHD), for up to 24 months, the above data image shows the effect of LUM-201 on increasing the pulsatile release of growth hormone (GH) in children with GHD (blue line on graph) compared to their baseline (grey line on graph) in a small study set. The study illustrates that small increases in GH area under the curve (AUC) from baseline are sufficient to stimulate an increase in growth. Likewise, it informs the impact of our Predictive Enrichment Marker (PEM) strategy to select for potentially responsive patients (PEM positive), as the PEM negative patient did not respond to treatment. These data have prompted our ongoing OraGrowtH212 Trial to explore increases in growth hormone pulsatility induced by LUM-201 at higher doses and in a larger cohort.
The OraGrowtH Phase 3 Trial is a Multicenter, 12-Month, Randomized, Double Blind, Placebo-Controlled Phase 3 Efficacy and Safety Study of Daily Oral LUM-201 in Naïve-to-Treatment, Prepubertal Children with Growth Hormone Deficiency (GHD).
The sponsor of this research study is Lumos Pharma, LLC and the NCT Identifier Number of the Trial is NCT06948214.
*IMPORTANT SAFETY INFORMATION: LUM-201 has a favorable investigational safety profile to date. LUM-201 was generally well-tolerated in children with the most commonly reported adverse events being increased appetite, pain in extremity and arthralgia. No meaningful safety signals have been observed in laboratory values, adverse events data, or in EKG values to date- Phase 2 Trials OraGrowtH210 and 212 Safety Data as of March 2024 cut-off date.
Click here for detailed information about the OraGrowtH Phase 3 Trial on the website called “ClinicalTrials.gov” managed by the United States Department of Health and Human Services.
GHD INFORMATIONAL SOURCES
https://rarediseases.org/rare-diseases/growth-hormone-deficiency
https://rarediseases.info.nih.gov/diseases/6552/growth-hormone-deficiency
SELECTED PUBLICATIONS
- George M Bright, MD
- Minh-Ha T Do, PhD
- John C McKew, PhD
- Werner F Blum, MD
- Michael O Thorner, MB, BS, DSc
Journal of the Endocrine Society, Volume 5, Issue 6, June 2021, bvab030
- Werner F Blum, MD
- George M Bright, MD
- Minh-Ha T Do, PhD
- John C McKew, PhD
- Haiying Chen, MD, PhD
- Michael O Thorner, MB, BS, DSc
Journal of the Endocrine Society, Volume 5, Issue 6, June 2021, bvab029
REFERENCES
1. Rosenfeld, R. et al, Compliance and Persistence in Pediatric and Adult Patients Receiving Growth Hormone Therapy, Endocrine Practice, 2008, 14(2):143-154
2. Cutfield, W.S. et al, Non-Compliance with Growth Hormone Treatment in Children Is Common and Impairs Linear Growth, PLOS ONE, 2011, 6(1): e16223
3. Lindsay Journal of Pediatrics, 1994, 125(1):29-35